Blog
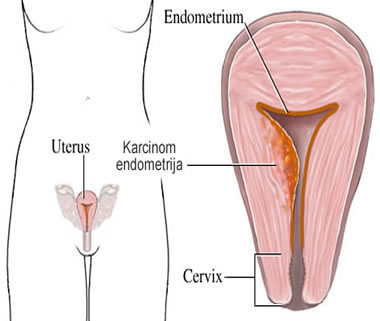
Endometrial cancer
After cancer of the breast, lungs and colon, endometrial cancer (cancer of the body of the uterus) ranks fourth in cancer of the female population. In 2000, 189,000 people died of endometrial cancer in the world and 44,700 women died.
The incidence rate is three times higher in developed countries. Numerous risk factors, directly or indirectly, endogenously or exogenously, lead to an increase in the number of women suffering from enometrial cancer. The tendency to prolong the life expectancy of the population has probably increased the incidence of this disease. The use of combination oral contraceptives reduces the risk of endometrial cancer disease by 30%, while progesterone pills alone reduce it even more significantly. Compared to this group, women who use unpaired estrogen (usually conjugated) for three years or more are five times more likely to have endometrial cancer. The use of intrauterine cartridges - a helix as a cause of endometrial cancer has not been proven. Endometrial cancer is one of the rarest causes of death with only 1.3% of deaths from malignancies in total. Such a low mortality rate is associated with the fact that almost 80% of endometrial cancer is diagnosed in the first stage of the disease. In recent years, there has been a slight increase in mortality caused by endometrial cancer
Etiology and risk factors
Long-term exposure to the unpowered action of estrogen is of great importance, whether endogenous or exogenous. People at risk include overweight (peripheral conversion of androgens to estrone in adipose tissue), women who did not give birth (reduced exposure to pregnancy-dominant progesterone), women with early menarche and late menopause (prolonged exposure to estrogens), patients polycystic ovary syndrome (increased LH - increased androgens and their conversion to estrone), patients with type II diabetes, suffering from estrogenic gonad tumors, and risk factors include history of tamoxifen, breast or ovarian cancer, and pelvic radiation. Low-risk groups are multiples and women who take oral contraceptives in the winter. Fiber-rich diets have a protective effect on endometrial cancer.
Diagnosis of endometrial cancer
Histological verification of the endometrial specimen is the only sure method of diagnosis. Ultrasound in the diagnosis of endometrial cancer. The morphological and vascular properties of the endometrium are studied by transvaginal ultrasound. Endometrial thickness over 14 mm in premenopausal and over 5 mm in postmenopausal are indicative of exploratory curettage, especially in women consuming hormone therapy or on tamoxifen therapy. Cytology in the diagnosis of endometrial cancer. Unlike cervical cancer and its precursors, cervical cytology is not sensitive enough to detect endometrial cancer. The reasons are anatomical and physiological: • as they pass through the worm duct into the vagina, the endometrial cells change degenerately and are difficult to recognize,
• due to postmenopausal cervical canal stenosis, endometrial cells are not in the cervical-vaginal smear or are small,
• well-differentiated adeno-carcinomas, as opposed to poorly differentiated ones, rarely spontaneously desquamate,
• there are differential diagnostic difficulties in distinguishing atypical endocervical cells from atypical endometrial cells.
Fractional curettage in diagnostics
Fractional curettage is the "gold standard" in the diagnosis of pathological endometrium. It is obligatory for: postmenopausal bleeding (when the endometrium is more than 4 mm thick), premenopausal bleeding and irregular bleeding of women over 35, postmenopausal women with pyometra, and suspected cytological and ultrasound findings. In 30% of postmenopausal women, bleeding occurs as a result of taking estrogen preparations, in 30% due to atrophic endometrium, 10% due to cervical or endometrial polypia, 10% due to other causes (cervical cancer, uterine sarcoma), 5% due to endometrial hyperplasia, and 15 % of postmenopausal bleeding is caused by endometrial cancer.
Endometrial hyperplasia — Endometrial hyperplasia is called the varying degrees of proliferation of the uterine mucosa that occurs in response to prolonged estrogen action without the suppressive action of progesterone.
Tamoxifen and the risk of endometrial cancer
While tamoxifen has cytostatic effects on breast cancer cells, it also promotes endometrial cancer cell growth. For 1,000 women who have taken tamoxifen for less than 5 years, 2-3 new cancers occur, and 13 new cancers for women who have taken tamoxifen between 6 and 7 years, which is why treatment with tamoxifen longer than 5 years is not recommended. An increased incidence of endometrial polpia in tamoxifen-treated women has been described. The average thickness of endometrium in patients treated with tamoxifen is 10.4 mm and any irregular uterine bleeding must be evaluated by fractional curettage.
Types of endometrial cancer
There is an absolute and relative increase in endometrial cancer, which is the most common malignant tumor of female genital organs in developed countries today. The likelihood that they will become ill during their lifetime exists in 2-3% of the female population. In 5% of cases, it occurs before the age of 40, about 25% of cases occur in premenopause, with the highest number between the ages of 50-65. There are two types of this disease:
Type I - estrogen dependent - occurs in women who have well-differentiated risk factors (diabetes, liver disease, high blood pressure, obesity, infertility, menstrual disorders), and in women treated with estrogens. Risk factors are related to hyperestrinism, that is, to the non-responsive action of endogenous or exogenous estrogen. This type of cancer develops in pre- and perimenopause, is well-differentiated, is often associated with different types of hyperplasia and estrogen and progesterone receptors are high. Histologically, these are subtypes with a favorable prognosis. Metastases and recurrences are rare
Type II - estrogen-independent - occurs in late postmenopausal women who have given birth, have a neat menstrual cycle, who are thin and have a neat endocrine-metabolic status. Histologically these are types with poor prognosis.
The prognosis of endometrial cancer is influenced by: clinical stage, histologic type and degree of maturity, depth of invasion and penetration into vascular spaces, involvement of cervix, adnexa and lymph nodes, steroid receptor status, DNA ploidy and increased expression of p53 genes.
Treatment of endometrial cancer
Endometrial cancer treatment is operative: isolated or combined with gestagen or cytostatic, or radiation.
Five-year survival of patients
Treated for ca.endometry
Stage of the disease Survival
Stage I 70 to 95%
Stage II 66 to 70%
Stage III 35 to 44%
Stage IV 14 to 20%
 34
34
 1500
1500
 5
5